Pain is a fundamental human experience, typically serving as a clear warning sign of injury. A stubbed toe or a sprained ankle hurts, but the cause is obvious, and the pain fades as the body heals. But for millions of people around the world, pain has no immediate or clear cause. This persistent, unexplainable, and often debilitating sensation is known as neuropathic pain, a condition that has plagued doctors and patients alike for decades. It’s a cruel paradox: the nervous system, meant to detect pain, becomes the very source of it. Now, groundbreaking new research focusing on a small, long-overlooked brain receptor called GluD1 is shedding light on the molecular mechanisms behind this suffering, offering a glimpse of a future where treatments might finally be able to repair, not just mask, the pain signals that have gone haywire.
The Unseen Burden of Neuropathic Pain
Neuropathic pain is fundamentally different from the kind of pain we experience from an injury. It stems not from physical damage, but from a malfunction within the nervous system itself. The condition is widespread and affects roughly 10% of the U.S. population, a number that continues to grow as the population ages. While it is often a complication of chronic conditions like diabetes or the result of chemotherapy and spinal cord injuries, its underlying biology remains poorly understood, making it incredibly difficult for doctors to treat effectively. Patients often describe a haunting, phantom pain that feels like burning, stabbing, or electricity, even from something as innocuous as a gentle breeze.
The impact of this chronic suffering extends far beyond the physical. Neuropathic pain takes a profound toll on mental health, often leading to severe depression, anxiety, and social isolation. The deep sense of helplessness that comes with living with an invisible and relentless condition can make even the most routine tasks feel unbearable. The economic burden is also staggering, contributing to billions of dollars in health care spending and lost productivity. In their desperate search for relief, many people turn to opioids, a path that has led to a devastating addiction crisis, highlighting the urgent need for a new generation of non-addictive, targeted therapies.
GluD1: The Molecular Architect of Pain
To find a better way to treat this ghost pain, scientists must first answer a series of fundamental questions. Why does the nervous system misfire in this way? What causes it to rewire itself to increase pain sensitivity? And most importantly, is it possible to reset the entire system? The answer may lie in a protein that has been largely ignored by the scientific community: a receptor called GluD1, short for glutamate delta-1 receptor.
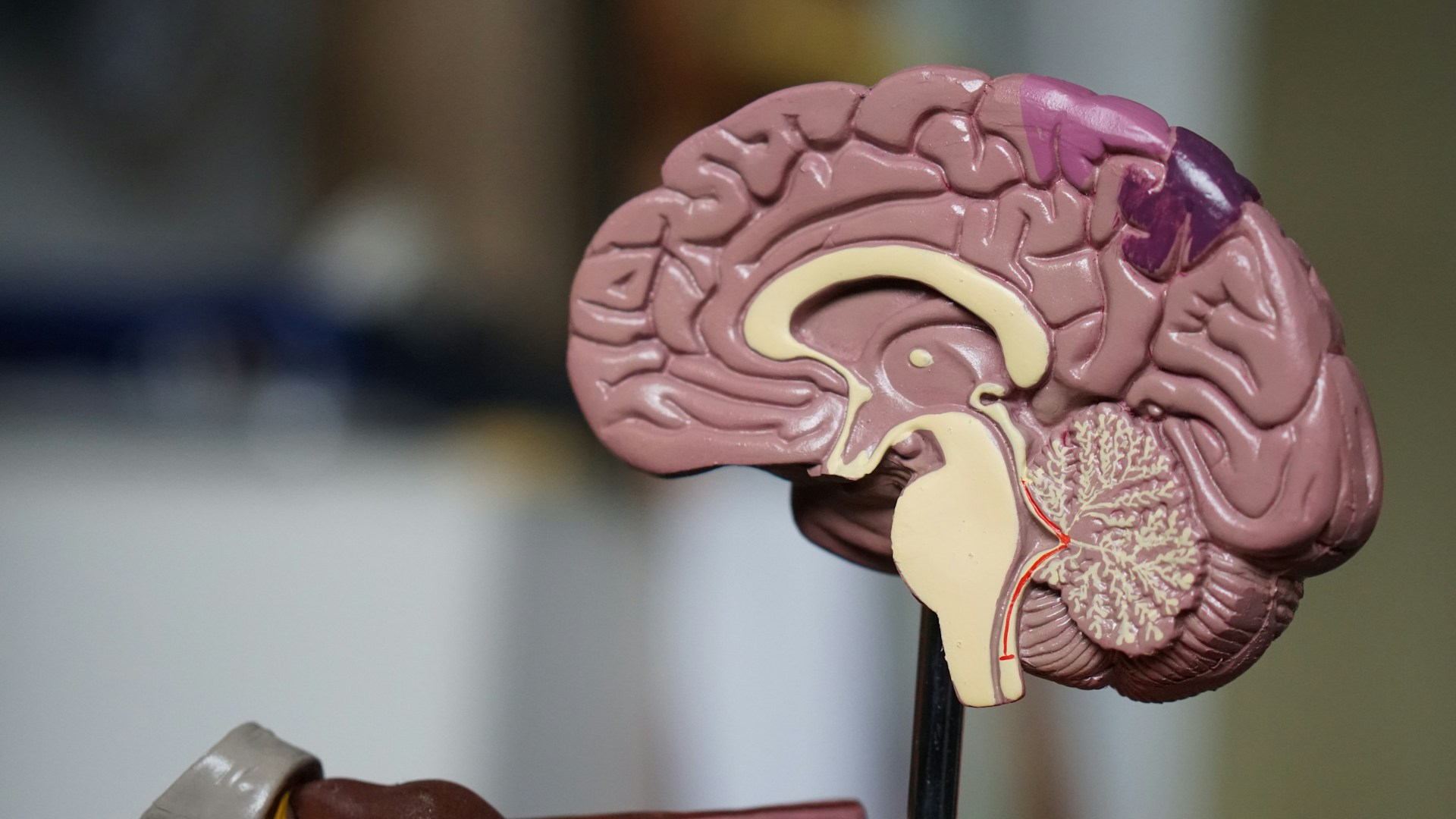
For years, scientists considered GluD1 to be a biochemical curiosity, not a key player in the transmission of electrical signals like its relatives in the glutamate receptor family. However, new research is revealing its true importance. Instead of transmitting messages, GluD1 acts as a molecular architect, helping to organize and shape the synapses—the crucial junctions where neurons connect and communicate. Think of it as a construction foreman, quietly directing where and how connections are formed. This organizing role is particularly critical in regions of the nervous system involved in processing pain and emotion, like the spinal cord and the amygdala, where GluD1 may be shaping how people experience pain both physically and emotionally.
A Broken Bridge and a New Hope

Further research has uncovered a critical mechanism involving GluD1. It has been found to work in tandem with another protein called cerebellin-1, and together they form a structure known as a trans-synaptic bridge. This bridge acts like a strong handshake between two neurons, ensuring that pain signals are appropriately processed and filtered. It is this stable connection that prevents the nervous system from becoming overwhelmed by sensory input.
However, in conditions of chronic pain, this bridge becomes unstable and begins to fall apart. The result is a chaotic breakdown in communication. The neurons begin to misfire and overreact, much like a group chat where everyone is shouting at once and no clear message can get through. This synaptic noise turns up the brain’s pain sensitivity, suggesting that GluD1 is not just managing pain signals but is actively shaping the emotional and physical intensity of those signals. The question then becomes: could we restore this broken connection to fix the underlying problem?
From Lab to a Real-World Lifeline
In a groundbreaking study, researchers tested this very hypothesis. They injected mice with cerebellin-1 and observed that it successfully reactivated GluD1 activity. The result was a dramatic easing of chronic pain in the mice, with no sedative effects or other disruptions to nerve signals that are common with opioids. This suggests a new path forward: instead of simply numbing the body to pain, reactivating GluD1 activity could recalibrate how the brain processes it. This new approach could potentially offer a way to heal the nervous system itself, with fewer side effects and less risk of addiction than current treatments.
Of course, this research is still in its early stages and a long way from human clinical trials. But the implications are immense and incredibly exciting. For the millions of people living with debilitating neuropathic pain, this small, unassuming receptor may offer a way out of the shadows. It represents a new frontier in pain management, one that focuses on repairing the system rather than just masking its symptoms, promising a new kind of relief that is both powerful and sustainable.